Just In
- 1 hr ago

- 2 hrs ago

- 5 hrs ago

- 9 hrs ago

Don't Miss
- Movies
 When Rekha Talked About 'Drinking Binges, Taking Drugs & Being Impure': I've Been Lusting Like Hell
When Rekha Talked About 'Drinking Binges, Taking Drugs & Being Impure': I've Been Lusting Like Hell - Sports
 'It Would be Awesome': Rohit Sharma advocates for India vs Pakistan Bilateral Series with Special Condition
'It Would be Awesome': Rohit Sharma advocates for India vs Pakistan Bilateral Series with Special Condition - Technology
 Vivo V30e Launch Date in India set for May 2: Flipkart Availability Confirmed
Vivo V30e Launch Date in India set for May 2: Flipkart Availability Confirmed - Finance
 Rs 14/Share Dividend: Stockbroking Co To Consider Bonus Share, Shares Up 126% In 180-Days
Rs 14/Share Dividend: Stockbroking Co To Consider Bonus Share, Shares Up 126% In 180-Days - News
 Karnataka Weather Alert: Light Rains Likely In Bengaluru In Next 24 Hours, Check Latest Forecast
Karnataka Weather Alert: Light Rains Likely In Bengaluru In Next 24 Hours, Check Latest Forecast - Travel
 Journey From Delhi To Ooty: Top Transport Options And Attractions
Journey From Delhi To Ooty: Top Transport Options And Attractions - Education
 IIIT-Bangalore Introduces PG Diploma In Digital Product Design And Management
IIIT-Bangalore Introduces PG Diploma In Digital Product Design And Management - Automobiles
 Jawa Yezdi Expands Mega Service Camps To 32 New Cities, Focusing On Tier-II And Tier-III Regions
Jawa Yezdi Expands Mega Service Camps To 32 New Cities, Focusing On Tier-II And Tier-III Regions
What is Diabetes Skin Patch and How It Works
For decades now, a major part of diabetes management has been all about daily finger pricks to measure one's blood sugar. Before the glucometer was invented, diabetics would use daily urine samples to get a general estimate of their blood glucose range [1] . The information obtained used to be extremely vague and hence not much helpful.
However, the present generation would only be aware of the glucometers that can provide results within 5 seconds [2] . Today's mainstream technique of diabetes management is through the use of continuous glucose monitoring (CGM) [3] that are enabled to directly send the readings to one's smartphone every five minutes.
However, modern-day technology still needs daily finger pricks apart from the weekly insertion of sharp sensor-enabled needles for those using CGM. Ongoing researchers have paved way for a new technique which would make finger-pricking tests for diabetes a thing of the past now. Read on to know more about how a needle-less patch is being created that can measure and monitor blood sugar levels effectively.
Bloodless Diabetes Monitoring Through Adhesive Patches
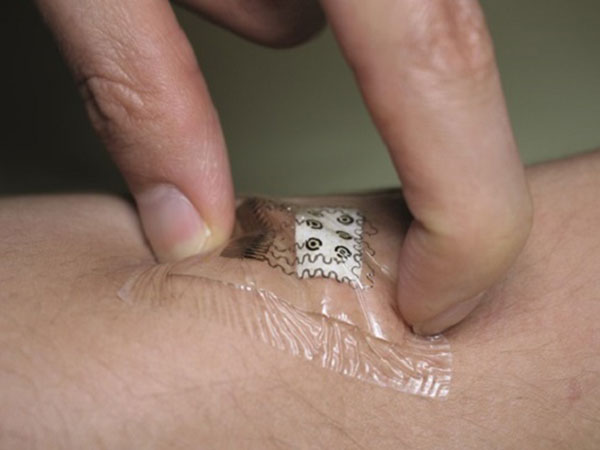
The creation of a non-invasive, adhesive patch promises the measurement of glucose levels through the skin without the need for a finger-prick blood test. This adhesive skin patch can measure glucose levels every 10 to 15 minutes [4] .
Type 2 diabetes is the most common form of diabetes (about 90 to 95 per cent of all cases). This kind of diabetes occurs when the body is no longer able to use insulin effectively or if there is a failure in producing enough of the hormone (causing blood glucose levels to become very high).
The researchers (who had been extensively working on the creation of this blood-less glucose monitoring method) have reported their findings and they seem quite favourable to be used by all diabetic patients.
Why The Finger-Prick Tests Are A Burden
To effectively manage diabetes, one would need to keep their blood glucose levels under control and this requires regular monitoring. The present method that most diabetics use is measuring glucose levels through a blood glucose meter. A needle is used to prick your finger in order to release a drop of blood, which can be tested.
The frequency of the finger-pricks is dependent on the type of diabetes a person has. It is also dependent on the type of medication that one has been using. Nevertheless, for people with type 1 diabetes, daily testing - which can go up to 10 times per day, is common.
Some
people
can
find
the
need
to
keep
pricking
their
fingers
every
now
and
then
quite
burdensome.
Many
experts
and
researchers
have
come
out
with
data
that
shows
that
some
of
the
barriers
to
good
blood
glucose
control
are
the
cost
of
blood
test
strips,
fear
of
pain
and
needles
and
the
inconvenience
of
the
self-monitoring
process
[5]
.
These
findings
have
made
the
researchers
look
out
for
blood
glucose
monitoring
ways
that
can
be
noninvasive
in
nature.
The
creators
of
the
new
diabetes
skin
patch
claim
that
this
invention
has
the
potential
to
change
the
face
of
blood
glucose
monitoring.
How The Diabetes Skin Patch Works
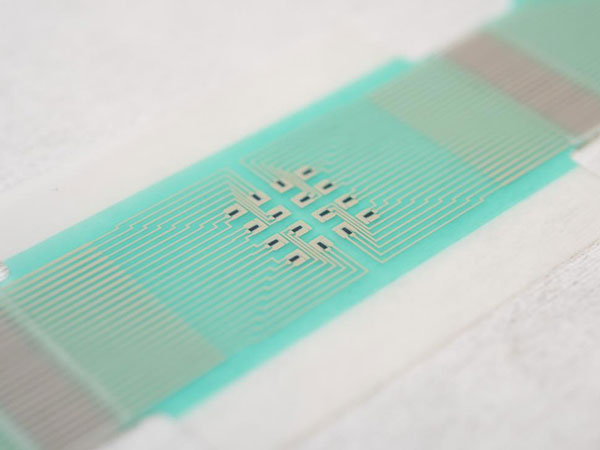
The adhesive skin patch is made of miniature sensors that use electric currents to obtain the glucose from the fluid that is secreted from hair follicles or cells. The skin patch is designed with tiny reservoirs that store the collected glucose, according to a study published in the journal Nature Nanotechnology [6] .
This is then used to measure the levels every 10 to 15 minutes. The idea behind this is making the patient get access to his or her glucose reading instantly. The readings can be sent to a user's smartphone or smartwatch. This also works in a great way to inform the user when he or she needs to have the diabetes medication.
The best part is that the adhesive patch does not pierce the skin. Such patches are highly accurate as they measure glucose from a very small area on hair follicles. The miniature sensors are capable of operating on a small area over an individual hair follicle. The levels obtained are accurate as inter-skin and intra-skin variability in glucose extraction is minimized [7] . The readings, therefore, do not require any confirmation with the use of blood sampling.
Researchers have used graphene as one of the components so that attributes such as being conductive, flexible and strong can be added to the new invention alongside the features of being potentially low-cost and environmentally friendly [8] . Experts have said that the design of the skin patch is such that it opens up possibilities of new creative additions to its existing internal as well as external look and working style. The design can be implemented using high-throughput fabrication techniques such as screen printing.
Researchers conducted trials on a set of people to confirm that glucose tracking was accurate and that levels were displayed correctly each time. Research is still underway to make an enhancement to this creation by increasing the number of sensors present (in order to increase accuracy further).

On A Final Note...
The powerful and innovative design of the skin patch using an array of sensors and reservoirs, have made the patch efficient in not requiring calibration with a blood sample. Thus making finger-pricking blood tests absolutely unnecessary. Researchers strongly believe that the skin patches are the future of effective diabetes management by serving to be a low-cost, wearable sensor [9] that is enabled to regularly send accurate glucose measurements to the wearer's smartphone or smartwatch.
Nonetheless, it is a good idea to hold back and wait until researchers completely give a green signal to the use of these skin patches. Few studies have reported that this creation still seems incomplete in a few ways. Although the skin patches have shown promising results when tested on human participants, yet there is a clearance of few clinical trials still pending, one of them being the demonstration of its full functionality over a 24-hour period [10] .
- [1] Marsden, J., & Pickering, D. (2015). Urine testing for diabetic analysis.Community eye health,28(92), 77.
- [2] Muktabhant, B., Sanchaisuriya, P., Sarakarn, P., Tawityanon, W., Trakulwong, M., Worawat, S., & Schelp, F. P. (2012). Use of glucometer and fasting blood glucose as screening tools for diabetes mellitus type 2 and glycated haemoglobin as a clinical reference in rural community primary care settings of a middle-income country.BMC public health,12, 349.
- [3] Pandit K. (2012). Continuous glucose monitoring.Indian journal of endocrinology and metabolism,16(Suppl 2), S263-266.
- [4] Sobel, S. I., Chomentowski, P. J., Vyas, N., Andre, D., & Toledo, F. G. (2014). Accuracy of a Novel Noninvasive Multisensor Technology to Estimate Glucose in Diabetic Subjects During Dynamic Conditions.Journal of diabetes science and technology,8(1), 54-63.
- [5] Bowman, F. B. (1938). PAINLESS, BLOODLESS, AND SAFE HÆMORRHOIDECTOMY.Canadian Medical Association journal,38(5), 430.
- [6] Roe, J. N., & Smoller, B. R. (1998). Bloodless glucose measurements.Critical Reviews™ in Therapeutic Drug Carrier Systems,15(3).
- [7] Klonoff, D. C. (1997). Noninvasive blood glucose monitoring.Diabetes care,20(3), 433-437.
- [8] Pu, Z., Zou, C., Wang, R., Lai, X., Yu, H., Xu, K., & Li, D. (2016). A continuous glucose monitoring device by graphene modified electrochemical sensor in microfluidic system.Biomicrofluidics,10(1), 011910.
- [9] Lodwig, V., & Heinemann, L. (2003). Continuous glucose monitoring with glucose sensors: calibration and assessment criteria.Diabetes technology & therapeutics,5(4), 572-586.
- [10] Roe, J. N., & Smoller, B. R. (1998). Bloodless glucose measurements.Critical Reviews™ in Therapeutic Drug Carrier Systems,15(3).
-
 healthExclusive: World Oral Health Day 2024: Doctor Shares How Diabetic Patients Can Maintain Their Oral Health
healthExclusive: World Oral Health Day 2024: Doctor Shares How Diabetic Patients Can Maintain Their Oral Health -
 healthWhat Is VIP? It Is Not What You Think! This One Is Connected To Blood Glucose, Here's What You Need To Know
healthWhat Is VIP? It Is Not What You Think! This One Is Connected To Blood Glucose, Here's What You Need To Know -
 pregnancy parentingWhat Are The 4 Must Have Vitamins For Kids With Diabetes?
pregnancy parentingWhat Are The 4 Must Have Vitamins For Kids With Diabetes? -
 healthDoes This Everyday Cooking Ingredient Trigger Diabetes?
healthDoes This Everyday Cooking Ingredient Trigger Diabetes? -
 healthRoller Coaster Effect In Diabetes: Why Does My Blood Sugar Level Go Up And Down, How To Stop It
healthRoller Coaster Effect In Diabetes: Why Does My Blood Sugar Level Go Up And Down, How To Stop It -
 healthSinger Shakira Loves These 2 Indian Sweets! How To Make It Diet-Friendly?
healthSinger Shakira Loves These 2 Indian Sweets! How To Make It Diet-Friendly? -
 healthWorld Diabetes Day 2023: 3 Weird Things That Can Put You At Risk Of Developing Diabetes
healthWorld Diabetes Day 2023: 3 Weird Things That Can Put You At Risk Of Developing Diabetes -
 healthWorld Diabetes Day 2023: Daily Habits That Make One At Risk Of Diabetes
healthWorld Diabetes Day 2023: Daily Habits That Make One At Risk Of Diabetes -
 wellnessWorld Diabetes Day 2023: Avoid These Common Mistakes When Testing Blood Sugar Levels
wellnessWorld Diabetes Day 2023: Avoid These Common Mistakes When Testing Blood Sugar Levels -
 healthDiwali 2023: Kalakand Recipe For Diabetic People; It Is Sugar-Free & Keto-Friendly
healthDiwali 2023: Kalakand Recipe For Diabetic People; It Is Sugar-Free & Keto-Friendly -
 healthHow Poor Air Quality During Can Raise Your Diabetes Risk
healthHow Poor Air Quality During Can Raise Your Diabetes Risk -
 healthWhip Up These 3 Diwali Sweets For Your Diabetic Mom Over 40
healthWhip Up These 3 Diwali Sweets For Your Diabetic Mom Over 40


 Click it and Unblock the Notifications
Click it and Unblock the Notifications



