Latest Updates
-
 Arjun Tendulkar Marries Saaniya Chandhok In Grand Mumbai Wedding; First Pics Go Viral
Arjun Tendulkar Marries Saaniya Chandhok In Grand Mumbai Wedding; First Pics Go Viral -
 UK07 Rider Anurag Dobhal Shares Emotional Video, Alleges Harassment After Inter-Caste Marriage
UK07 Rider Anurag Dobhal Shares Emotional Video, Alleges Harassment After Inter-Caste Marriage -
 How a Blockbuster Ignited a Popcorn Boom: The Dhurandhar Effect and the Rise of Gourmet Cinema Snacks in India
How a Blockbuster Ignited a Popcorn Boom: The Dhurandhar Effect and the Rise of Gourmet Cinema Snacks in India -
 Splitsvilla X6 Episode 25 OTT Release: Tejasswi Prakash’s Cameo, Karan Calls Her His Real-Life Ideal Match
Splitsvilla X6 Episode 25 OTT Release: Tejasswi Prakash’s Cameo, Karan Calls Her His Real-Life Ideal Match -
 Rashmika and Vijay Deverakonda’s Hyderabad Reception: Decoding the Looks, Moments, And Who Came
Rashmika and Vijay Deverakonda’s Hyderabad Reception: Decoding the Looks, Moments, And Who Came -
 Horoscope for Today March 05, 2026 - Small Habits, Big Daily Wins
Horoscope for Today March 05, 2026 - Small Habits, Big Daily Wins -
 Holi 2026: The Aftercare Routine Your Skin And Hair Will Thank You For
Holi 2026: The Aftercare Routine Your Skin And Hair Will Thank You For -
 Over-Scrubbing After Holi? You Could Be Damaging Your Skin Microbiome, Not Just Removing Colour
Over-Scrubbing After Holi? You Could Be Damaging Your Skin Microbiome, Not Just Removing Colour -
 Horoscope for Today March 04, 2026 - Practical Steps for Calm Wins
Horoscope for Today March 04, 2026 - Practical Steps for Calm Wins -
 Happy Holi 2026 Wishes: 50+ Colourful Quotes, Messages, Status And Posts For WhatsApp, Facebook And Instagram
Happy Holi 2026 Wishes: 50+ Colourful Quotes, Messages, Status And Posts For WhatsApp, Facebook And Instagram
Peripartum Cardiomyopathy: What You Should Know
Very rarely, during or after pregnancy, a mother can develop a type of heart condition called peripartum cardiomyopathy. Peripartum cardiomyopathy (PPCM) is a rare kind of heart failure that happens during the last month of pregnancy or within five months after delivery.
The term 'cardiomyopathy' refers to heart muscle disease. Peripartum cardiomyopathy is also referred to as 'postpartum cardiomyopathy'. It is a rare condition with mild or severe symptoms.

In peripartum cardiomyopathy, the heart chambers enlarge and the heart muscle weakens. This causes a decrease in percentage of blood ejected from the left ventricle of the heart, with each contraction, thereby resulting in reduced blood flow, and the heart is unable to meet the demands of the body organs for oxygen. This affects the liver, lungs, and other body systems.

What Causes Peripartum Cardiomyopathy?
Generally, the heart pumps 50 per cent more blood during pregnancy, as there is increased need of transferring oxygen and vital nutrients to the developing baby. Although there is no definite cause for peripartum cardiomyopathy, one reason as suggested by the doctors is when this additional pumping of blood, is combined with few other risk factors that places additional stress on the heart.

Such risk factors may include
• Having previous pregnancies with similar condition
• Viral illness
• Low immunity
• Small-vessel disease
• Genetics
• Coronary artery spasm
• Poor nutrition
• Obesity
• Certain medications
• Advanced maternal age (women over 30 or 35 years of age)
• Preeclampsia
• Smoking and alcoholism

Symptoms Of Peripartum Cardiomyopathy
The symptoms of peripartum cardiomyopathy are similar to that of heart failure. You may experience the following common symptoms:
• Rapid heartbeat or palpitation
• Severe fatigue
• Chest pain
• Shortness of breath
• Tiredness during physical activity
• Increased urination, particularly at night
• Swollen feet and ankles

How Is It Diagnosed?
Your doctor can listen to any crackling noises in the lungs or abnormal sounds in the heart using a stethoscope. Your blood pressure may also be monitored.
Several imaging tests are done to measure your heart and determine the rate of blood flow. These tests include chest X-ray, CT scan of the heart, nuclear heart scan, and echocardiogram.
Laboratory tests are also part of the evaluation. Tests to assess kidney, liver and thyroid functioning, and to assess sodium and potassium, and a complete blood count to look for anaemia or infection is done. Further, markers of cardiac injury and stress may also be used to assess levels of risk.
The seriousness of the condition is measured by ejection fraction, based on the percentage of blood the heart pumps out with each beat. Normal ejection fraction number is about 60 per cent.

Treatment Options
Early diagnosis is the most effective treatment. Therefore, heightened suspicion is important when a pregnant woman comes in with signs of heart failure, as early diagnosis can help in getting the treatment started early on.
It is better to begin with standard heart failure therapy in case of peripartum cardiomyopathy, making use of available protocols.
The treatment for peripartum cardiomyopathy involves keeping extra fluid from getting collected in the lungs and to help the heart recover as completely as possible. Several women recover normal heart function and stabilize on medicines. Rarely, in some cases, it may progress to severe heart failure, requiring mechanical support or heart transplantation.
In majority of the cases, the physician prescribes treating symptoms with safe medications during pregnancy or for women who are breastfeeding. Doctors may also recommend a low-salt diet, daily weighing, or fluid restrictions. Smoking or drinking alcohol should be stopped completely, as they can worsen symptoms.
A heart biopsy may help to determine the underlying cause of cardiomyopathy, but the procedure is uncommon.

Lifestyle Modifications
Some lifestyle modifications can help reduce the risk, especially for first-time mothers. So the focus should be on the following:
Regular exercise (mild form of exercise that is not too strenuous)
Eating low-fat diet
Avoid all kinds of junk foods
Avoid smoking and alcohol
Remain relaxed and stress-free
Include prayer, yoga and meditation in your routine

What Are The Complications Involved?
Depending on the severity, generally, women who develop this condition during pregnancy may have their hearts returning to normal post-delivery. But for some, their condition may continue to worsen, and in such cases a heart transplant may be necessary.
Severe complications of peripartum cardiomyopathy may include arrhythmia (irregular heartbeat), blood clots in the lungs, congestive heart failure and death.
If you have experienced peripartum cardiomyopathy, then discuss with your doctor about possible complications before going ahead with a second pregnancy. This is because for patients with left ventricular dysfunction, if it fails to normalize during follow-up, the risk of further deterioration is higher during subsequent pregnancies, and this may pose danger to the life of the mother.


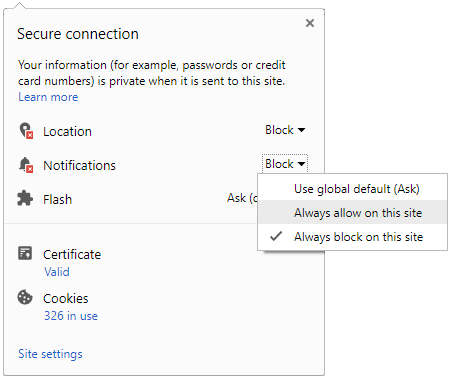
 Click it and Unblock the Notifications
Click it and Unblock the Notifications