Just In
- 5 hrs ago

- 6 hrs ago

- 7 hrs ago

- 7 hrs ago

Don't Miss
- Education
 West bengal class 12th Result 2024 Tentative Date: West Bengal class 12th 2024 Result Expected Soon on wbresul
West bengal class 12th Result 2024 Tentative Date: West Bengal class 12th 2024 Result Expected Soon on wbresul - Movies
 Razakar Review: Makrand Deshpande Film Makes Bold Attempt To Touch Sensitive Topic Of Hyderabad Genocide
Razakar Review: Makrand Deshpande Film Makes Bold Attempt To Touch Sensitive Topic Of Hyderabad Genocide - Automobiles
 Toyota Fortuner Leader Edition – Top Things You Need To Know
Toyota Fortuner Leader Edition – Top Things You Need To Know - Sports
 'I Spend Rs 85 lakh in my holidays': Virender Sehwag tells Adam Gilchrist how he refused BBL offer
'I Spend Rs 85 lakh in my holidays': Virender Sehwag tells Adam Gilchrist how he refused BBL offer - News
 RBI's Order To Kotak Mahindra Bank: No New Customers, No New Credit Cards
RBI's Order To Kotak Mahindra Bank: No New Customers, No New Credit Cards - Technology
 HMD Branded First Set of Android Smartphones Are Here!
HMD Branded First Set of Android Smartphones Are Here! - Finance
 Vodafone Idea FPO: Shares To Debut Tomorrow; GMP Hints Premium Listing; Shares Slump 9%
Vodafone Idea FPO: Shares To Debut Tomorrow; GMP Hints Premium Listing; Shares Slump 9% - Travel
 Mumbai Opens BMC Headquarters For Exclusive Heritage Tour
Mumbai Opens BMC Headquarters For Exclusive Heritage Tour
Sneddon Syndrome: Causes, Symptoms, Diagnosis & Treatment
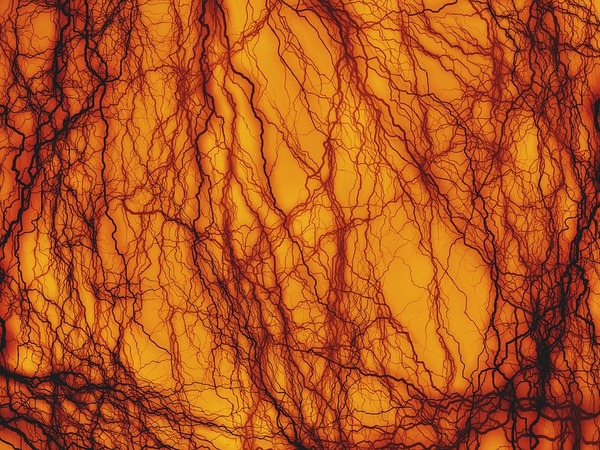
Sneddon syndrome is a rare and progressive condition that affects your blood vessels. It causes ischemic strokes in young adults and is a form of arteriopathy [1] . According to medical professionals, the condition is characterised by a disease of the small to medium-sized arteries which can cause an elevation in the chances of blood clots developing in the arteries; especially the arteries that supply to the skin and brain).
The condition causes the development of livedo reticularis, which are net-like patterns of discolouration on the skin as well as neurological abnormalities. Most cases of Sneddon syndrome are sporadic, however, familial cases associated with autosomal dominant inheritance have also been reported [2] , [3] .
Sneddon syndrome is often categorised into two different types depending on whether an underlying cause has been identified (primary versus idiopathic), or whether certain symptoms of the autoimmune disease are present or not (aPL-positive versus aPL negative).
The condition is also termed as livedo reticularis racemosa and cerebrovascular accidents and Sneddon's syndrome [4] .
Symptoms Of Sneddon Syndrome
The signs of the condition vary in accordance with its severity as well as the areas in your body that are affected by the syndrome. The condition is primarily recognised by the most common symptoms, which are, livedo reticularis, net-like patterns of discolouration on the skin and neurological abnormalities. According to studies, the average age for the onset of neurological symptoms is 39 years and livedo can develop from 29 years [5] .
The symptoms include the following [6] :
- Transient ischemic attack (TIA)
- Headache
- Seizures
- Skin discolouration (livedo racemosa), most commonly on the arms and legs, buttocks, trunk, face, hands, and feet
- Depression
- Changes in behaviour
- Stroke
- Dementia
- Dizziness
- Reduced intellectual ability
- Memory loss
- Psychiatric disturbances
- Vertigo
One of the most common symptoms of Sneddon syndrome is a stroke, which is a severe one too. You can identify the onset of stroke through the following signs [7] :
- Sudden, severe headache with no known cause
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden trouble walking
- Sudden confusion
- Sudden trouble speaking
- Sudden trouble seeing in one or both eyes
- Sudden dizziness, loss of balance or coordination
In women, it can develop some specific signs such as [8]
- Face, arm or leg pain
- Hiccups or nausea
- Chest pain or palpitations
- Shortness of breath
In rare cases, the condition has been known to show the signs of Raynaud's phenomenon, which is a widespread and mottled-purple discolouration on the body [9] . And some of the others rare symptoms include chorea and myelopathies which are the disorders of the spinal cord, high blood pressure, heart disease, ophthalmologic (eye) complications, and impaired renal (kidney) function.
Causes Of Sneddon Syndrome
Studies have been unable to understand the exact reason behind the development of the condition. It is understood that Sneddon syndrome develops due to the changes in the CECR1 gene. The changes in the genes aid in producing the enzyme known as adenosine deaminase 2, which supports the lining of the blood vessel walls [10] .
In some cases, the syndrome is associated with autoimmune diseases such as systemic lupus erythematosus, antiphospholipid syndrome, Behçet disease, or mixed connective tissue disease.
Genetic factors are also asserted to play a role in causing Sneddon syndrome. It is pointed out to be a cause as there have been reports of familial cases. It has been reported that the syndrome can affect more than one family member, such as the occurrence of it being on siblings. A person can carry the gene or genes of the syndrome without having any symptoms, as the condition will only be activated or triggered under specific circumstances [11] .

Diagnosis Of Sneddon Syndrome
The examination of the condition is carried out through physical examinations. The doctor will examine the medical history as well as the symptoms of the individual. You need to go to a doctor immediately in the event of livedo racemosa (pattern of skin discolouration).
The most commonly used diagnostic methods for Sneddon syndrome are skin biopsy and genetic tests. The neurological symptoms such as unexplained stroke in young individuals will also be examined by the doctor so as to understand the root cause of the severe symptoms [12] .
Apart from these methods, the individual will have to undergo the following [13] :
- Blood tests
- Brain MRI which may reveal white matter changes, infarcts, microbleeds or atrophy
- A thorough cardiovascular evaluation
- Skin biopsy, which may reveal occlusion of arterioles by the proliferation of the inner lining
- Cerebral angiography, which is usually abnormal in up to 75% of patients
While conducting the blood tests to understand the symptoms, it will be used to examine the presence of the following [14] :
- Lupus anticoagulant
- Antithrombin-III
- Protein c or protein s
- Circulating immune complexes
- Anti-nuclear (ana) and anti-double-stranded DNA autoantibodies
- Thrombocytopenia and leukopenia, which is low white cell count
- Vdrl
- Cryoglobulins
- Immunoglobulin igg and possibly IgM anti-cardiolipin antibodies, that is, the types of antiphospholipid antibodies, which may be positive in about 60% of cases
Treatment For Sneddon Syndrome
As there is no cure developed for the condition, the treatment plans focus on managing the symptoms of the patient. The rare nature of the disease can be attributed to the lack of treatment methods developed. It is also the reason behind the lack of clinical studies conducted to further explore the condition and formulate a cure for it [15] .
The treatment methods adopted for Sneddon syndrome are through blood thinning or anticoagulant medications such as warfarin. It helps in minimising the risk of stroke. If the individual is suffering from uncontrolled high blood pressure or diabetes or has the habit of smoking - the treatment methods will focus on dealing with those too. Some doctors suggest that it is preferable for patients who are aPL-negative to adopt methods that are lesser aggressive such as an approach consisting of antiplatelet therapy with aspirin [16] , [17] .
Angiotensin-converting enzyme (ACE) inhibitors are also employed as it can reduce the growth of the inside lining of the vessels (endothelial proliferation). Prostaglandin is employed to improve gas exchange and blood flow in the small vessels [18] .
Refrain from smoking and oestrogen oral contraceptives as it can control the severity of the neurological symptoms [19] , [20] .
- [1] Tietjen, G. E., Al-Qasmi, M. M., Gunda, P., & Herial, N. A. (2006). Sneddon's syndrome: another migraine-stroke association?. Cephalalgia, 26(3), 225-232.
- [2] Tietjen, G. E., Al‐Qasmi, M. M., & Shukairy, M. S. (2002). Livedo reticularis and migraine: a marker for stroke risk?. Headache: The Journal of Head and Face Pain, 42(5), 352-355.
- [3] Bolayir, E., Yilmaz, A., Kugu, N., Erdogan, H., Akyol, M., & Akyuz, A. (2004). Sneddon's syndrome: clinical and laboratory analysis of 10 cases. Acta medica Okayama, 58(2), 59-66.
- [4] Tietjen, G. E., Gottwald, L., Al‐Qasmi, M. M., Gunda, P., & Khuder, S. A. (2002). Migraine is associated with livedo reticularis: a prospective study. Headache: The Journal of Head and Face Pain, 42(4), 263-267.
- [5] Bruyn, R. P. M., Van der Veen, J. P. W., Donker, A. J. M., Valk, J., & Wolters, E. C. (1987). Sneddon's syndrome: case report and literature review. Journal of the neurological sciences, 79(3), 243-253.
- [6] Stockhammer, G., Felber, S. R., Zelger, B., Sepp, N., Birbamer, G. G., Fritsch, P. O., & Aichner, F. T. (1993). Sneddon's syndrome: diagnosis by skin biopsy and MRI in 17 patients. Stroke, 24(5), 685-690.
- [7] Rehany, U., Kassif, Y., & Rumelt, S. (1998). Sneddon's syndrome: neuro-ophthalmologic manifestations in a possible autosomal recessive pattern. Neurology, 51(4), 1185-1187.
- [8] Zelger, B., Sepp, N., Stockhammer, G., Dosch, E., Hilty, E., Öfner, D., ... & Fritsch, P. O. (1993). Sneddon's syndrome: a long-term follow-up of 21 patients. Archives of dermatology, 129(4), 437-447.
- [9] Menzel, C., Reinhold, U., Grünwald, F., Von Smekal, A., Uerlich, M., Rieker, O., ... & Biersack, H. J. (1994). Cerebral blood flow in Sneddon syndrome. Journal of Nuclear Medicine, 35, 461-461.
- [10] Adair, J. C., Digre, K. B., Swanda, R. M., Hartshorne, M. F., Lee, R. R., Constantino, T. M. E., & Knoefel, J. E. (2001). Sneddon's syndrome: a cause of cognitive decline in young adults. Cognitive and Behavioral Neurology, 14(3), 197-204.
- [11] Gondim, F. D. A. A., Leacock, R. O., Subrammanian, T. A., & Cruz-Flores, S. (2003). Intracerebral hemorrhage associated with Sneddon's syndrome: is ischemia-related angiogenesis the cause? Case report and review of the literature. Neuroradiology, 45(6), 368-372.
- [12] Bersano, A., Morbin, M., Ciceri, E., Bedini, G., Berlit, P., Herold, M., ... & Savoiardo, M. (2016). The diagnostic challenge of Divry van Bogaert and Sneddon Syndrome: Report of three cases and literature review. Journal of the neurological sciences, 364, 77-83.
- [13] Jonathan, C., Shelley, R., Mario, T., & Philip, C. (2018). WED 253 An atypical presentation of sneddon syndrome.
- [14] Rutter-Locher, Z., Chen, Z., Flores, L., Basu, T., Creamer, D., Weeks, R., ... & Nashef, L. (2016). Sneddon's syndrome: it is all in the ectoderm. Practical neurology, 16(4), 300-303.
- [15] Nagai, N., Ohta, Y., Izumi‐Nagai, K., Shinoda, H., Tsubota, K., & Ozawa, Y. (2016). Sneddon's syndrome with optic disc macroaneurysm and macular edema successfully treated with subtenon steroid injection. Acta ophthalmologica, 94(6), e517.
- [16] de Amorim, L. C. D., Maia, F. M., & Rodrigues, C. E. M. (2017). Stroke in systemic lupus erythematosus and antiphospholipid syndrome: risk factors, clinical manifestations, neuroimaging, and treatment. Lupus, 26(5), 529-536.
- [17] Forchhammer, S., Metzler, G., & Ghoreschi, K. (2018). Long-term follow-up of early-onset Sneddon syndrome: A case report. JAAD case reports, 4(9), 880-882.
- [18] Collantes-Rodríguez, C., Jiménez-Gallo, D., Arjona-Aguilera, C., Ossorio-García, L., & Linares-Barrios, M. (2016). Treatment of skin ulcers secondary to sneddon syndrome with alprostadil (Prostaglandin E1). JAMA dermatology, 152(6), 726-727.
- [19] Fierini, F., Barilaro, A., Giambene, B., Carlucci, G., Grandi, V., Maio, V., & Pantoni, L. (2015). Moyamoya in a patient with Sneddon’s syndrome. Clin Neurol Neurosurg, 129, 34-6.
- [20] Forchhammer, S., Metzler, G., & Ghoreschi, K. (2018). Long-term follow-up of early-onset Sneddon syndrome: A case report. JAAD case reports, 4(9), 880-882.
-
 pregnancy parentingWhite Lung Syndrome: What Are The Symptoms Of The Disease Rampant In China? How Does It Spread?
pregnancy parentingWhite Lung Syndrome: What Are The Symptoms Of The Disease Rampant In China? How Does It Spread? -
 healthWhat Is Traffic Stress Syndrome? Are You At Risk?
healthWhat Is Traffic Stress Syndrome? Are You At Risk? -
 disorders cureWhat Is Jerusalem Syndrome? A Psychosis State That Makes People Hear ‘Voices Of Angels’
disorders cureWhat Is Jerusalem Syndrome? A Psychosis State That Makes People Hear ‘Voices Of Angels’ -
 disorders cureWhat Is Alice in Wonderland Syndrome (AWS)? Causes, Symptoms And Treatment
disorders cureWhat Is Alice in Wonderland Syndrome (AWS)? Causes, Symptoms And Treatment -
 disorders cureWhat Is Refeeding Syndrome? Its Symptoms, Risk Factors And Treatment
disorders cureWhat Is Refeeding Syndrome? Its Symptoms, Risk Factors And Treatment -
 disorders cureRestless Leg Syndrome: Symptoms, Causes, Diagnosis And Treatment
disorders cureRestless Leg Syndrome: Symptoms, Causes, Diagnosis And Treatment -
 disorders cureCompartment Syndrome: Causes, Symptoms, Diagnosis And Treatment
disorders cureCompartment Syndrome: Causes, Symptoms, Diagnosis And Treatment -
 disorders cureGoodpasture Syndrome (GPS): Causes, Symptoms, Diagnosis And Treatment
disorders cureGoodpasture Syndrome (GPS): Causes, Symptoms, Diagnosis And Treatment -
 babyGrey Baby Syndrome: Causes, Symptoms, Diagnosis and Treatment
babyGrey Baby Syndrome: Causes, Symptoms, Diagnosis and Treatment -
 prenatalTwin-to-twin Transfusion Syndrome - Everything you need to know
prenatalTwin-to-twin Transfusion Syndrome - Everything you need to know -
 healthWorld HIV/AIDS Day: What Is The Difference Between HIV and AIDS?
healthWorld HIV/AIDS Day: What Is The Difference Between HIV and AIDS? -
 healthDengue 101: Causes, Symptoms, Risks, Complications, Treatment, Prevention, Diet And More
healthDengue 101: Causes, Symptoms, Risks, Complications, Treatment, Prevention, Diet And More


 Click it and Unblock the Notifications
Click it and Unblock the Notifications



