Just In
- 32 min ago

- 8 hrs ago

- 17 hrs ago

- 18 hrs ago

Don't Miss
- Finance
 1:10 Split Coming Up: Crorepati FMCG ITC Turns Rs 1,50,000 To Rs 1.2 Crore; Makes Big Announcement; BUY?
1:10 Split Coming Up: Crorepati FMCG ITC Turns Rs 1,50,000 To Rs 1.2 Crore; Makes Big Announcement; BUY? - Sports
 Pakistan vs New Zealand Playing 11: PAK vs NZ 4th T20I Team News, Predicted Lineup And Other Details
Pakistan vs New Zealand Playing 11: PAK vs NZ 4th T20I Team News, Predicted Lineup And Other Details - Education
 JEE Main Result 2024 Out, Telangana's 15 Toppers Shine, Check Statewise List of 56 Candidates with Perfect 100
JEE Main Result 2024 Out, Telangana's 15 Toppers Shine, Check Statewise List of 56 Candidates with Perfect 100 - News
 Mangalsutra Row: Did Indira Gandhi Donate Gold During The 1962 War? The Facts Behind Priyanka's Claim
Mangalsutra Row: Did Indira Gandhi Donate Gold During The 1962 War? The Facts Behind Priyanka's Claim - Movies
 Kota Factory 3 OTT Release Date, Platform: When Will Jitendra Kumar's Web Series Premiere On Netflix?
Kota Factory 3 OTT Release Date, Platform: When Will Jitendra Kumar's Web Series Premiere On Netflix? - Travel
 Escape to Kalimpong, Gangtok, and Darjeeling with IRCTC's Tour Package; Check Itinerary
Escape to Kalimpong, Gangtok, and Darjeeling with IRCTC's Tour Package; Check Itinerary - Technology
 OPPO Find X7 Ultra Camera Deep-Dive: Pushing the Boundaries of Photography on a Smartphone
OPPO Find X7 Ultra Camera Deep-Dive: Pushing the Boundaries of Photography on a Smartphone - Automobiles
 Aston Martin Vantage Launched In India At Rs 3.99 Crore
Aston Martin Vantage Launched In India At Rs 3.99 Crore
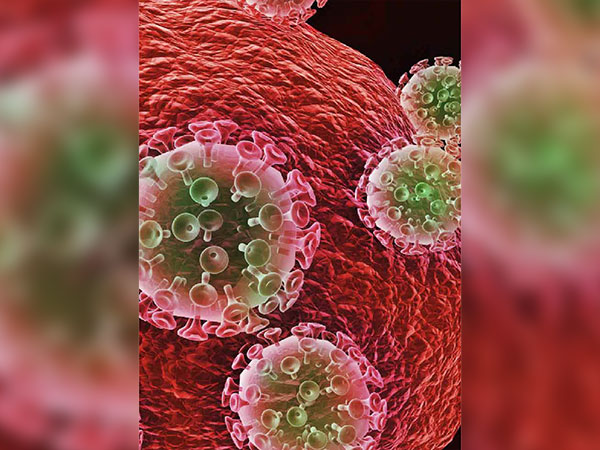
HAART (Highly Active Antiretroviral Therapy) For Treating HIV
The discovery of HIV in 1981 brought along with it a variety of drug therapies. 'One drug therapy' was initially used to treat people living with AIDS. The most common drug used in the early days was AZT. Although it was initially successful, such form of 'monotherapies' was ultimately found to be ineffective in slowing down the progression of the AIDS-causing virus [1] .
The failure of monotherapies was attributed to the fact that HIV had the ability to quickly create resistance to single-drug treatments. HIV was able to mutate into a form wherein it stopped responding to the individual drugs being administered [2] .

A combination drug treatment was discovered in 1995. This was known as 'AIDS cocktail'. This therapy was later renamed and is now known as 'Highly Active Antiretroviral Therapy (HAART). It is sometimes also called Combination Antiretroviral Therapy (cART) or simply Antiretroviral Therapy (ART) [3] .
HAART has shown dramatic improvements in the life of people with AIDS. There has been a decrease in the amount of HIV in the body with the use of this treatment. Studies also show an increase in the count of CD4 cells (immune cells that HIV destroys) [4] .
Read on to know more about the life-changing treatment called HAART.
What Is HAART?
HAART
is
the
acronym
for
'Highly
Active
Antiretroviral
Therapy'.
The
term
was
coined
in
the
late
1990s,
keeping
in
mind
the
effectiveness
of
this
combination
drug
therapy
in
treating
HIV
[5].
In
1996,
with
the
introduction
of
protease
inhibitors
[6]
,
doctors
combined
three
or
more
drug
agents
in
such
a
way
that
it
could
successfully
stop
HIV
from
replicating
at
different
points
in
its
life
cycle.
Studies
show
that
with
the
use
of
HAART,
a
startling
50
per
cent
reduction
in
AIDS-related
deaths
were
observed
[7]
.
HAART is also popularly known as 'triple therapy' and 'triple drug cocktail'. This therapy is a customized combination of different medicine classes that a doctor ideally prescribes considering factors such as patient's viral load (amount of virus in the blood), the CD4+ cell count, the particular strain of the virus, etc. However, one should note that HAART cannot get rid of HIV from one's body, and therefore it must be taken by the patient for the rest of his or her life [8] .
HAART basically aims at controlling the viral load and delays/prevents the onset of symptoms and the progression to AIDS. It, therefore, is able to prolong the survival of the people who are infected with HIV.
HAART is known to have effectively managed this ailment which was once concluded as a fatal condition.
How Is HIV Detected?
When a person has contracted HIV, the immune system starts producing antibodies that are nothing but proteins which recognize the virus. The tests conducted to diagnose HIV are basically tests that detect the presence of these antibodies. A brief period of about 6 to 8 weeks after being exposed to the virus is required for the tests to detect and give results accurately.
Although many new test methodologies claim that it can be reduced to a window of just 2 weeks [9] . This waiting period (before tests start showing positive results) is believed to be the most complex and dangerous for HIV transmission. This is so because the chances of a false negative test result are high during this period and yet the person might be highly infectious (spreading the virus rapidly through unsafe actions). The Centers for Disease Control and Prevention (CDC) has now recommended the inclusion of HIV testing as a part of routine medical care for anyone between 13 and 64 years of age [10] .
How HAART Works
Unlike the single-drug or drug-drug therapies, the combination of three or more antiretroviral (as in HAART) drugs are capable of effectively suppressing a wide range of HIV that might be present in a single viral population. When three or more drugs are combined, even if one drug is unable to suppress a particular kind of viral type then the other drug agents come into action [11] .
When the viral population is kept suppressed (not detectable), then there would only be few circulating viruses in the bloodstream and hence fewer opportunities for the virus to mutate into a resistance strain [12] .
This approach of HAART therapy is what became the foundation of its success, unlike the pre-HAART therapies. The therapies that were deployed prior to HAART failed because smaller mutant population were permitted to persist. This eventually increased in number and became the predominant viral strain. When this happened, the drugs were no longer able to stop HIV from replicating [13] (a condition referred to as 'drug resistant')

Drugs Used In HAART
At present, there are five classes of antiretroviral drugs. Each drug is responsible for suppressing a specific stage in the life cycle of HIV. The five classes are as follows [14] :
Entry or fusion inhibitors (includes CCR5 receptor antagonists)
- These inhibitors are designed to prevent the virus from entering the CD4 cells.
Nucleoside and nucleotide reverse transcriptase inhibitors (NRTI/NtRTI)
- For HIV to replicate, it requires an enzyme known as reverse transcriptase (RT) [15] . NRTIs blocks the virus's ability to replicate by offering faulty versions of RT to the viruses.
Non-nucleoside reverse transcriptase inhibitors (NNRTI)
- These work by disabling a key protein which HIV requires to replicate
Integrase inhibitors (INSTI)
- When HIV enters the CD4 cells, it inserts genetic material into the cells. This insertion is made possible due to the assistance provided by a protein called integrase [16] . The INSTIs are designed to block the virus's ability to complete the replication step.
Protease inhibitors (PI)
- A protein called protease [17] (key building block that is essential for HIV to replicate) is disabled by this inhibitor.
Investigations are underway for other classes of antiretrovirals. The newer generation drugs are being developed with the aim to improve tolerability, simplify dosing for those on therapy and reduce adverse effects [18] .
Recommended HIV Treatment Protocol
Going by what the National Institutes of Health suggests, the current recommended dosage for initial HIV drug regimen includes three HIV medicines from two or more different classes of drugs. It usually is of the following kind [19] :
- Two NRTIs along with an INSTI, NNRTI or PI
- cobicistat or ritonavir as a booster
Once put on a regimen, it is the responsibility of the doctor to thoroughly monitor the patient and keep a check on the ongoing reaction and success levels. If the regimen does not seem to work or in case the patient starts to show allergic reactions/side effects, then the healthcare provider would need to make changes to the drug regimen.
All people living with HIV are recommended antiretroviral treatment. However, in some cases, receiving treatment is more of an emergency. Such situations could be when [20] :
- the person is pregnant [21]
- the person has previously experienced HIV-related dementia or cancer (including other HIV-related complications such as nerve pain or infection)
- the person has had CD4 counts that are below 200 cells/mm3 [22]
- the person has hepatitis B or hepatitis C
Continuing antiretroviral treatment life long ensures a low viral load and normal CD4 count, thus ensuring the longer survival of a person infected with HIV [23] .
The Future Of HAART
Apart from just being used as a form of suppression for individuals infected with HIV, HAART is also finding use in being deployed for the reversal of infection rates in the high-risk population. This strategy is termed as 'Treatment as Prevention (TasP)' [24] . Studies have shown that this strategy is quite effective in reducing the 'community viral load' within a particular population. This has made it difficult for the virus to be passed on from an infected person to a non-infected person.
Moreover, research is being widely conducted to determine the effectiveness of HAART in not just reducing risks of HIV, but also that of non-HIV-related illnesses, such as heart diseases and cancer. Medical experts recommend that HAART is initiated in all persons with HIV, irrespective of the geographic region, race, HIV viral load, immune status or income.
The concept of HAART is going to be further modified with the introduction of long-lasting antiretroviral drug agents (which would facilitate monthly or quarterly injections) and next-generation drugs [25] . The aim of these newly developed drugs would be to lower the traditional triple-drug cocktail to fewer drugs (maybe just two).
- [1] Broder S. (2009). The development of antiretroviral therapy and its impact on the HIV-1/AIDS pandemic. Antiviral research, 85(1), 1-18.
- [2] Heredia, A., Hassounah, S., Medina-Moreno, S., Zapata, J. C., Le, N. M., Han, Y., Foulke, J. S., Davis, C., Bryant, J., Redfield, R. R., … Wainberg, M. A. (2017). Monotherapy with either dolutegravir or raltegravir fails to durably suppress HIV viraemia in humanized mice. The Journal of antimicrobial chemotherapy, 72(9), 2570-2573.
- [3] Heredia, A., Hassounah, S., Medina-Moreno, S., Zapata, J. C., Le, N. M., Han, Y., Foulke, J. S., Davis, C., Bryant, J., Redfield, R. R., … Wainberg, M. A. (2017). Monotherapy with either dolutegravir or raltegravir fails to durably suppress HIV viraemia in humanized mice. The Journal of antimicrobial chemotherapy, 72(9), 2570-2573.
- [4] Lifson, A. R., Krantz, E. M., Eberly, L. E., Dolan, M. J., Marconi, V. C., Weintrob, A. C., Crum-Cianflone, N. F., Ganesan, A., Grambsch, P. L., Agan, B. K., Infectious Disease Clinical Research Program (IDCRP) HIV Working Group (2011). Long-term CD4+ lymphocyte response following HAART initiation in a U.S. Military prospective cohort. AIDS research and therapy, 8(1), 2.
- [5] Delaney M. (2006). History of HAART – the true story of how effective multi-drug therapy was developed for treatment of HIV disease. Retrovirology, 3(Suppl 1), S6.
- [6] Lv, Z., Chu, Y., & Wang, Y. (2015). HIV protease inhibitors: a review of molecular selectivity and toxicity. HIV/AIDS (Auckland, N.Z.), 7, 95-104.
- [7] Mayer, K. H., & Venkatesh, K. K. (2010). Antiretroviral therapy as HIV prevention: status and prospects. American journal of public health, 100(10), 1867-1876.
- [8] Lima, V. D., Harrigan, R., Bangsberg, D. R., Hogg, R. S., Gross, R., Yip, B., & Montaner, J. S. (2009). The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. Journal of acquired immune deficiency syndromes (1999), 50(5), 529-536.
- [9] Fearon M. (2005). The laboratory diagnosis of HIV infections. The Canadian journal of infectious diseases & medical microbiology = Journal canadien des maladies infectieuses et de la microbiologie medicale, 16(1), 26-30.
- [10] Sands A. Diagnostics for HIV diagnosis. In: Consolidated Guidelines on HIV Testing Services: 5Cs: Consent, Confidentiality, Counselling, Correct Results and Connection 2015. Geneva: World Health Organization; 2015 Jul. ANNEX 7.
- [11] El Bouzidi, K., Collier, D., Nastouli, E., Copas, A. J., Miller, R. F., & Gupta, R. K. (2016). Virological efficacy of PI monotherapy for HIV-1 in clinical practice. The Journal of antimicrobial chemotherapy, 71(11), 3228-3234.
- [12] Sánchez, M. S., Grant, R. M., Porco, T. C., & Getz, W. M. (2006). HIV drug-resistant strains as epidemiologic sentinels. Emerging infectious diseases, 12(2), 191-197.
- [13] Häggblom, A., Santacatterina, M., Neogi, U., Gisslen, M., Hejdeman, B., Flamholc, L., & Sönnerborg, A. (2017). Effect of therapy switch on time to second-line antiretroviral treatment failure in HIV-infected patients. PloS one, 12(7), e0180140.
- [14] Kemnic TR, Gulick PG. HIV, Antiretroviral Therapy. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-.
- [15] Coffin JM, Hughes SH, Varmus HE, editors. Retroviruses. Cold Spring Harbor (NY): Cold Spring Harbor Laboratory Press; 1997. Overview of Reverse Transcription.
- [16] Craigie R. (2012). The molecular biology of HIV integrase. Future virology, 7(7), 679-686.
- [17] López-Otín, C., & Bond, J. S. (2008). Proteases: multifunctional enzymes in life and disease. The Journal of biological chemistry, 283(45), 30433-30437.
- [18] Zhang X. (2018). Anti-retroviral drugs: current state and development in the next decade. Acta pharmaceutica Sinica. B, 8(2), 131-136.
- [19] Bhatti, A. B., Usman, M., & Kandi, V. (2016). Current Scenario of HIV/AIDS, Treatment Options, and Major Challenges with Compliance to Antiretroviral Therapy. Cureus, 8(3), e515.
- [20] Mayer, K. H., & Venkatesh, K. K. (2010). Antiretroviral therapy as HIV prevention: status and prospects. American journal of public health, 100(10), 1867-76.
- [21] Kastner, J., Matthews, L. T., Flavia, N., Bajunirwe, F., Erikson, S., Berry, N. S., & Kaida, A. (2014). Antiretroviral Therapy Helps HIV-Positive Women Navigate Social Expectations for and Clinical Recommendations against Childbearing in Uganda. AIDS research and treatment, 2014, 626120.
- [22] Ying, R., Granich, R. M., Gupta, S., & Williams, B. G. (2016). CD4 Cell Count: Declining Value for Antiretroviral Therapy Eligibility. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 62(8), 1022-8.
- [23] Freedberg, K. A., & Sax, P. E. (2016). Improving on effective antiretroviral therapy: how good will a cure have to be?. Journal of medical ethics, 43(2), 71-73.
- [24] Hull, M. W., & Montaner, J. S. (2013). HIV treatment as prevention: the key to an AIDS-free generation. Journal of food and drug analysis, 21(4), S95-S101.
- [25] Lichterfeld, M., & Zachary, K. C. (2011). Treating HIV-1 Infection: What Might the Future Hold?. Therapeutic advances in chronic disease, 2(5), 293-305.
-
 astrologyWorld AIDS Day 2023: Messages, Slogans, Wishes And Quotes Of Hope, And Compassion
astrologyWorld AIDS Day 2023: Messages, Slogans, Wishes And Quotes Of Hope, And Compassion -
 healthWorld HIV/AIDS Day: Ancient AIDS Treatments: Did They Stand the Test of Time?
healthWorld HIV/AIDS Day: Ancient AIDS Treatments: Did They Stand the Test of Time? -
 healthWorld HIV/AIDS Day: What Is The Difference Between HIV and AIDS?
healthWorld HIV/AIDS Day: What Is The Difference Between HIV and AIDS? -
 healthWorld AIDS Day: 3 Not So Common Ways HIV Can Spread from Person to Person
healthWorld AIDS Day: 3 Not So Common Ways HIV Can Spread from Person to Person -
 pregnancy parenting14 Children Infected With HIV, Hepatitis After Blood Transfusion In UP Hospital: How Did It Happen?
pregnancy parenting14 Children Infected With HIV, Hepatitis After Blood Transfusion In UP Hospital: How Did It Happen? -
 healthSexual Diseases You Might Have Without Symptoms
healthSexual Diseases You Might Have Without Symptoms -
 pulseZero Discrimination Day 2023: Date, Theme, And Why It Is Observed
pulseZero Discrimination Day 2023: Date, Theme, And Why It Is Observed -
 disorders cureWorld AIDS Day 2022: Can Kissing An HIV Positive Person Cause An HIV Infection?
disorders cureWorld AIDS Day 2022: Can Kissing An HIV Positive Person Cause An HIV Infection? -
 wellnessHIV Positive Patients In Haryana To Get Free Health Facilities Like Lab And Radiological Tests
wellnessHIV Positive Patients In Haryana To Get Free Health Facilities Like Lab And Radiological Tests -
 kidsCipla, DNDi Launch 4-In-1 Antiretroviral Treatment For Children With HIV
kidsCipla, DNDi Launch 4-In-1 Antiretroviral Treatment For Children With HIV -
 disorders cureNew Study Signals The Development Of Unique Genetic Treatment For HIV
disorders cureNew Study Signals The Development Of Unique Genetic Treatment For HIV -
 disorders cureOver 17 Lakh People Contracted HIV In India In Last 10 Years By Unprotected Sex: RTI Reply
disorders cureOver 17 Lakh People Contracted HIV In India In Last 10 Years By Unprotected Sex: RTI Reply


 Click it and Unblock the Notifications
Click it and Unblock the Notifications



