Just In
- 6 hrs ago

- 7 hrs ago

- 10 hrs ago

- 17 hrs ago

Don't Miss
- Sports
 Most Wickets In IPL 2024, Purple Cap Holder: Top 10 And Teamwise Top 5 Wicket-Takers On April 20
Most Wickets In IPL 2024, Purple Cap Holder: Top 10 And Teamwise Top 5 Wicket-Takers On April 20 - Finance
 2:1 Bonus Issue: IT Penny Stock Turned; 1,600 Shares Market Lot Size Revised To 4,800 Shares
2:1 Bonus Issue: IT Penny Stock Turned; 1,600 Shares Market Lot Size Revised To 4,800 Shares - Movies
 Bigg Boss Malayalam 6 Voting Trends: Saranya, Sreerekha or Jaanmoni; Who Will Get Least Votes On Mohanlal’s Sh
Bigg Boss Malayalam 6 Voting Trends: Saranya, Sreerekha or Jaanmoni; Who Will Get Least Votes On Mohanlal’s Sh - News
 Chinese President Xi Jinping Orders Biggest Military Reorganisation Since 2015
Chinese President Xi Jinping Orders Biggest Military Reorganisation Since 2015 - Education
 Exam Pressure Does Not Exist; Studying Punctually is Crucial; Says Aditi, the PSEB 2024 Topper
Exam Pressure Does Not Exist; Studying Punctually is Crucial; Says Aditi, the PSEB 2024 Topper - Automobiles
 Suzuki Swift Hatchback Scores 4 Star Safety Rating At JNCAP – ADAS, New Engine & More
Suzuki Swift Hatchback Scores 4 Star Safety Rating At JNCAP – ADAS, New Engine & More - Technology
 Dell Introduces AI-Powered Laptops and Mobile Workstations for Enterprises in India
Dell Introduces AI-Powered Laptops and Mobile Workstations for Enterprises in India - Travel
 Journey From Delhi To Ooty: Top Transport Options And Attractions
Journey From Delhi To Ooty: Top Transport Options And Attractions
Periodontitis: Symptoms, Causes, Risk factors, Treatment And Prevention
Periodontitis is the advanced form of a gum infection in which the gums and bones that surround the teeth are damaged due to bacterial infection which results from poor oral hygiene. The condition often causes loosening of the teeth, tooth fall and other health complications [1] .
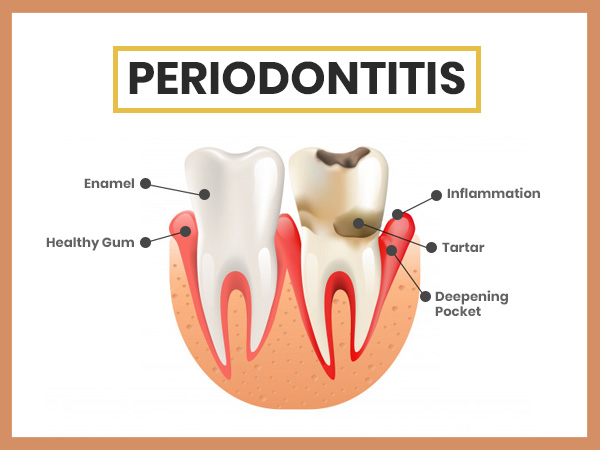
Our gums and teeth are full of bacteria which are harmless until they grow in numbers due to poor oral hygiene. Whenever we eat, the tiny particles of the food get stuck in between the mouth allowing the bacteria to feed on it. This results in the formation of colourless and sticky plaque and tartar (mineralized plaque) on teeth.
When the plaque and tartar stay on teeth for longer, the bacteria multiply and cause gingivitis [2] . However, it is the mild form of gum disease and usually gets reversed by regular oral health maintenance. When gingivitis is left untreated, the harmful bacterial infection extends to the bone of the teeth and cause periodontitis, a serious form of the gum disease which often result in gum decay and loosening of the teeth [3] .

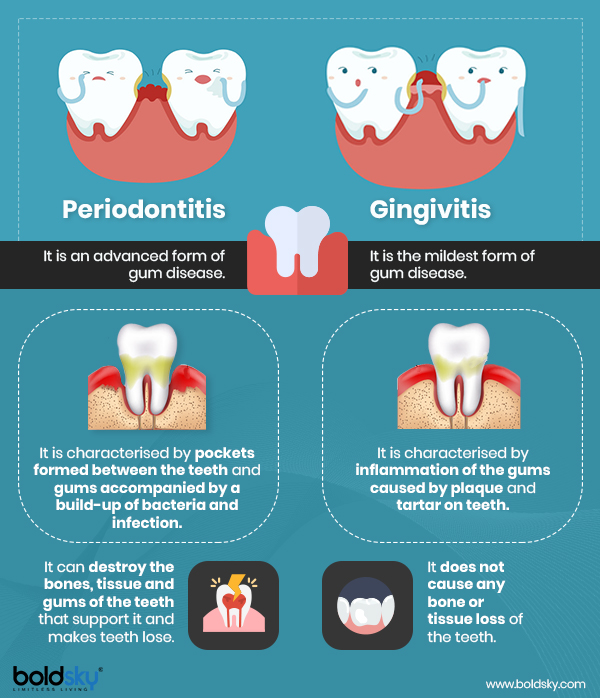
Difference Between Periodontitis And Gingivitis
Gingivitis and periodontitis are the two types of gum disease that differentiate in their stages of gum decay [3] . Let's see the difference between the two types.
Types Of Periodontitis
There are 3 types of periodontitis which are as follows:
1. Chronic periodontitis: It is the common form of periodontitis identified by chronic inflammation of the tissues that surround the teeth. The condition is caused due to accumulation of plaque and common in adults. However, it can be reversed with early treatment but gets worse if left untreated [4] .
2. Aggressive periodontitis: It occurs mainly in childhood but may affect younger adults. The condition causes the rapid destruction of tissues and bone around the teeth and results in early teeth loss if left untreated. It generally affects black and male teenagers compared to the white race and females [5] .
3. Necrotizing periodontal disease: The condition results in tissue necrosis (lack of blood supply) and infection caused due to the death of gum tissues, supporting bone and ligaments of the teeth. It occurs generally in people who have suppressed the immune system, like people with HIV or who are undergoing cancer treatment [6] .
Symptoms Of Periodontitis
The symptoms of periodontitis depend on the stage of the condition. The common symptoms of this gum infection are as follows:
- Bleeding gums while brushing or flossing [3] .
- Bad breath [7]
- Inflammation of the gums [8]
- Receding gums [3]
- Foul taste in the mouth
- Red and tender gums
- Plaque or yellowish of the teeth [2]
- Tartar or mineralized form of plaque on the teeth
- Pain while eating
- Loose teeth
Causes Of Periodontitis
Periodontitis is caused due to the negligence of oral hygiene. The concept is simple, if you don't clean your mouth properly, bacteria will build up and cause severe harm to the gums and bones of your teeth causing periodontitis. Here are the causes of periodontitis.
- Plaque: This is the first phase of gum disease. When a soft and sticky film starts building up on the teeth making it yellowish, it is a sign of plaque. The condition is caused when sugar and starch interact with thousands of bacteria present in the mouth [2] .
- Tartar (calculus): When plaque is left untreated, it gets hardened on the teeth making it difficult to remove by brushing or flossing. Tartar is basically a mass filled with bacteria that can cause severe gum diseases if left untreated for long [9] .
- Gingivitis: It is the severe form of plaque and tartar but mild form of periodontitis. Gingivitis result in inflammation and irritation of the gums present around the base of the teeth [10] .
The final stage of gingivitis causes periodontitis in which a pocket is formed between the gums and the teeth filled with bacteria, plaque and tartar.
Risk Factors Of Periodontitis
Several factors may increase the risk of periodontitis in a person. The risk factors are as follows:
- Smoking [11]
- Hormonal imbalance in women due to pregnancy, puberty and menopause [12] .
- Family history [13]
- Medicines that dry up the saliva formed in the mouth.
- Medical conditions that cause a decrease in immunity like cancer and AIDS [14]
- Stress [15]
- Older age [16]
- Substance abuse [17]
- Alcoholism [18]
- Gingivitis or poor oral hygiene [10]
- Deficiency of vitamin C [19]
- Inflammatory diseases like Crohn's disease, diabetes [20] and rheumatoid arthritis.
Coconut Oil For Teeth: Benefits And How To Use It
Complications Of Periodontitis
Studies suggest that the bacteria which cause periodontitis can enter our bloodstream through gums and cause other serious complications of the heart and lungs. However, there is very little evidence to prove the above fact. Some of the common complications of periodontitis are as follows:
Shifting of the teeth which may cause problem while eating.
- Painful abscesses [21]
- Complications during pregnancy that may result in low child weight and preeclampsia.
- Receding gums
Diagnosis Of Periodontitis
The diagnosis of this gum and bone disease of the teeth is carried out by the following processes.
- Medical history: To find out the cause behind the condition like smoking or medications that cause dry mouth.
- Mouth examination: To check for signs of plaque or tartar buildup, bleeding gums, swollen gums, loose teeth and receding gums [22] .
- Examining pocket depth: To know the severity of the condition by measuring the pocket depth by a periodontal probe.
- X-ray: To view the bone loss caused due to the formation of pocket between the gums and teeth.
Treatment Of Periodontitis
Treatment of periodontitis is carried out in 2 ways - non-invasive treatment which is recommended during the beginning phase of the condition and invasive treatment which is suggested when the gum disease reaches an advanced stage.
1. Noninvasive treatments
Scaling: To remove bacteria and tartar formed on the tooth surface by a laser or ultrasonic device [23] .
Antibiotics: They are in a form of antiseptic mouthwash, capsule, gel or tablets. They are helpful to kill stubborn bacteria and reduce the size of infected pockets [24] .
Root planing: A process to smoothe the root surfaces of the teeth and prevent further build-up of bacteria that cause inflammation, decay or loosening of the gums [25] .
2. Invasive treatments
Surgery: The surgery is performed to reduce the size of the periodontal pockets by making tiny incisions on the gum tissues to lift it. Also, if there's a bone loss due to periodontitis, first the bone is contoured and then the gum tissues are sutured back to place [3] .
Bone grafting: The process is performed when the damage is done to the bone around the tooth root. A piece of bone either from your body or from a donor is transplanted to the infected or missing bone area which further helps to regrow the natural bone [26] .
Tissue grafting: The process is used to stop receding of the gums and gum line. Here, a small portion of the healthy and soft tissue, either from your mouth or donor's mouth is transplanted in the infected area to cover the exposed roots and allow the formation of more healthy gums [27] .
How To Prevent Periodontitis
- Brush your teeth at least twice in a day; before the breakfast and after dinner.
- Buy an electric brush as it is more effective in removing plaque and tartar.
- Change your brush in every 3-4 months.
- Quit smoking and tobacco.
- If possible, clean your mouth with an antiseptic mouth wash and floss with a dental pick fter every meal to prevent plaque from between teeth.
- Visit a dentist every month.
- Get adequate sleep to reduce your stress.
- Eat a balanced diet to keep your immune system strong.
- [1] Saini, R., Marawar, P. P., Shete, S., & Saini, S. (2009). Periodontitis, a true infection. Journal of global infectious diseases, 1(2), 149–150. doi:10.4103/0974-777X.56251
- [2] Mehrotra N, Singh S. Periodontitis. [Updated 2019 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.
- [3] InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Gingivitis and periodontitis: Overview. 2011 Oct 5 [Updated 2014 Jun 18].
- [4] Agrali, O. B., & Kuru, B. E. (2015). Periodontal treatment in a generalized severe chronic periodontitis patient: A case report with 7-year follow-up. European journal of dentistry, 9(2), 288–292. doi:10.4103/1305-7456.156844
- [5] Roshna, T., & Nandakumar, K. (2012). Generalized aggressive periodontitis and its treatment options: case reports and review of the literature. Case reports in medicine, 2012, 535321. doi:10.1155/2012/535321
- [6] Bermejo-Fenoll, A., & Sánchez-Pérez, A. (2004). Necrotising periodontal diseases. Medicina Oral, Patología Oral y Cirugía Bucal, 9, 114-9.
- [7] Porter, S. R., & Scully, C. (2006). Oral malodour (halitosis). BMJ (Clinical research ed.), 333(7569), 632–635. doi:10.1136/bmj.38954.631968.AE
- [8] Khan, S. A., Kong, E. F., Meiller, T. F., & Jabra-Rizk, M. A. (2015). Periodontal Diseases: Bug Induced, Host Promoted. PLoS pathogens, 11(7), e1004952. doi:10.1371/journal.ppat.1004952
- [9] Checchi, L., D'Achille, C., & Montella, A. (1991). Tartar and periodontal disease--a cofactor in etiopathogenesis. Dental Cadmos, 59(8), 80-4.
- [10] Lang, N. P., Schätzle, M. A., & Löe, H. (2009). Gingivitis as a risk factor in periodontal disease. Journal of clinical periodontology, 36, 3-8.
- [11] Underner, M., Maes, I., Urban, T., & Meurice, J. C. (2009). Effects of smoking on periodontal disease. Revue des maladies respiratoires, 26(10), 1057-1073.
- [12] Soory, M. (2000). Hormonal factors in periodontal disease. Dental update, 27(8), 380-383.
- [13] Shearer, D. M., Thomson, W. M., Caspi, A., Moffitt, T. E., Broadbent, J. M., & Poulton, R. (2011). Inter-generational continuity in periodontal health: findings from the Dunedin family history study. Journal of clinical periodontology, 38(4), 301–309. doi:10.1111/j.1600-051X.2011.01704.x
- [14] Rajesh, K. S., Thomas, D., Hegde, S., & Kumar, M. S. (2013). Poor periodontal health: A cancer risk?. Journal of Indian Society of Periodontology, 17(6), 706–710. doi:10.4103/0972-124X.124470
- [15] Goyal, S., Gupta, G., Thomas, B., Bhat, K. M., & Bhat, G. S. (2013). Stress and periodontal disease: The link and logic!!. Industrial psychiatry journal, 22(1), 4–11. doi:10.4103/0972-6748.123585
- [16] Wu, Y., Dong, G., Xiao, W., Xiao, E., Miao, F., Syverson, A., … Graves, D. T. (2016). Effect of Aging on Periodontal Inflammation, Microbial Colonization, and Disease Susceptibility. Journal of dental research, 95(4), 460–466. doi:10.1177/0022034515625962
- [17] Saini, G. K., Gupta, N. D., & Prabhat, K. C. (2013). Drug addiction and periodontal diseases. Journal of Indian Society of Periodontology, 17(5), 587–591. doi:10.4103/0972-124X.119277
- [18] Tezal, M., Grossi, S. G., Ho, A. W., & Genco, R. J. (2001). The effect of alcohol consumption on periodontal disease. Journal of Periodontology, 72(2), 183-189.
- [19] Pussinen, P. J., Laatikainen, T., Alfthan, G., Asikainen, S., & Jousilahti, P. (2003). Periodontitis is associated with a low concentration of vitamin C in plasma. Clinical and diagnostic laboratory immunology, 10(5), 897–902. doi:10.1128/cdli.10.5.897-902.2003
- [20] Preshaw, P. M., Alba, A. L., Herrera, D., Jepsen, S., Konstantinidis, A., Makrilakis, K., & Taylor, R. (2012). Periodontitis and diabetes: a two-way relationship. Diabetologia, 55(1), 21–31. doi:10.1007/s00125-011-2342-y
- [21] Bhat, G. S., Singh, V., & Bhat, K. M. (2012). Recurrent periodontal abscess associated with "teeth as a tool". Journal of Indian Society of Periodontology, 16(1), 113–114. doi:10.4103/0972-124X.94617
- [22] Preshaw P. M. (2015). Detection and diagnosis of periodontal conditions amenable to prevention. BMC oral health, 15 Suppl 1(Suppl 1), S5. doi:10.1186/1472-6831-15-S1-S5
- [23] InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Gingivitis and periodontitis: Treatment of periodontitis: Cleaning, scaling, care. 2011 Oct 5 [Updated 2014 Jun 18].
- [24] Kapoor, A., Malhotra, R., Grover, V., & Grover, D. (2012). Systemic antibiotic therapy in periodontics. Dental research journal, 9(5), 505–515.
- [25] CADTH Rapid Response Reports. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2011-.
- [26] Gojkov-Vukelic, M., Hadzic, S., & Pasic, E. (2017). Evaluation of efficacy of surgical periodontal therapy with the use of bone graft in the treatment of periodontal intrabony defects. Medical Archives, 71(3), 208.
- [27] Sumer, M., Keles, G. C., Cetinkaya, B. O., Balli, U., Pamuk, F., & Uckan, S. (2013). Autogenous cortical bone and bioactive glass grafting for treatment of intraosseous periodontal defects. European journal of dentistry, 7(1), 6–14.
-
 wellness40 Best Superfoods To Maintain Oral Health
wellness40 Best Superfoods To Maintain Oral Health -
 healthHoli 2024: 5 Dental Tips For A Safer Holi So That You Have The Brightest Smile
healthHoli 2024: 5 Dental Tips For A Safer Holi So That You Have The Brightest Smile -
 healthHow Air Pollution Impacts Your Oral Health, Makes Your Mouth Dry And Damage Your Enamel, Know From An Expert
healthHow Air Pollution Impacts Your Oral Health, Makes Your Mouth Dry And Damage Your Enamel, Know From An Expert -
 healthHow Do You Give Oral Care To The Elderly? Tips And Tricks To Solve Dental Issues
healthHow Do You Give Oral Care To The Elderly? Tips And Tricks To Solve Dental Issues -
 healthDental Anxiety And Fear: Know The Causes And How To Communicate Your Fear
healthDental Anxiety And Fear: Know The Causes And How To Communicate Your Fear -
 healthIs Tongue Scraping Good For Oral Health?
healthIs Tongue Scraping Good For Oral Health? -
 healthTobacco Usage And Oral Health: How Does It Affect Your Mouth?
healthTobacco Usage And Oral Health: How Does It Affect Your Mouth? -
 healthHow Dental Digital Scans Is Revolutionizing Dentistry And Changing Dynamics In Dental Care
healthHow Dental Digital Scans Is Revolutionizing Dentistry And Changing Dynamics In Dental Care -
 healthWhat Is the Best Dental Implant Maintenance?
healthWhat Is the Best Dental Implant Maintenance? -
 healthHow To Choose Right Toothbrush For Your Teeth
healthHow To Choose Right Toothbrush For Your Teeth -
 healthCan Vitamin D Affect Oral Health?
healthCan Vitamin D Affect Oral Health? -
 healthIs Same Day Dental Implant Right For You? Know The Benefits
healthIs Same Day Dental Implant Right For You? Know The Benefits


 Click it and Unblock the Notifications
Click it and Unblock the Notifications



