Just In
- 2 hrs ago

- 3 hrs ago

- 6 hrs ago

- 6 hrs ago

Don't Miss
- Finance
 Rs 7.50/Share Dividend: Adani Group Cement Company Reports Strong Q4 Results; Profit Surges 2x YoY
Rs 7.50/Share Dividend: Adani Group Cement Company Reports Strong Q4 Results; Profit Surges 2x YoY - Movies
 Heeramandi Premiere: Newly Engaged Aditi Rao Hydari Dazzles In A Multi-Coloured Anarkali Set; Guess The PRICE
Heeramandi Premiere: Newly Engaged Aditi Rao Hydari Dazzles In A Multi-Coloured Anarkali Set; Guess The PRICE - Education
 Tamil Nadu SSLC Results 2024: Number of Ways you can check the Results
Tamil Nadu SSLC Results 2024: Number of Ways you can check the Results - News
 Rajnath Singh Or Nitin Gadkari Could Have Been PM: Mamata Banerjee's Dig At BJP
Rajnath Singh Or Nitin Gadkari Could Have Been PM: Mamata Banerjee's Dig At BJP - Automobiles
 Bajaj To Offer Chetak Electric Scooter At Lower Price Point: All Details Here
Bajaj To Offer Chetak Electric Scooter At Lower Price Point: All Details Here - Sports
 Bangladesh vs Zimbabawe: Will Shakib Al Hasan Play Home T20 Series In May Or Not?
Bangladesh vs Zimbabawe: Will Shakib Al Hasan Play Home T20 Series In May Or Not? - Technology
 Qualcomm Reveals Snapdragon X Plus Chip for Laptops: 10 Core CPU, On-Device AI, & Much More
Qualcomm Reveals Snapdragon X Plus Chip for Laptops: 10 Core CPU, On-Device AI, & Much More - Travel
 Escape to Kalimpong, Gangtok, and Darjeeling with IRCTC's Tour Package; Check Itinerary
Escape to Kalimpong, Gangtok, and Darjeeling with IRCTC's Tour Package; Check Itinerary
Necrotizing Fasciitis: Causes, Symptoms, Diagnosis, Treatment And Prevention
There has been a recent news report that states that a Michigan man passed away of 'flesh-eating' bacteria after he helped with the recovery of Hurricane Ian. Doctors have informed the media that Hewitt was infected with Vibrio Vulnificus bacteria, commonly known as the "flesh-eating bacteria.".
Previously, a 12-year-old girl from Florida was found fighting for her life after she had contracted a deadly flesh-eating disease known as 'necrotizing fasciitis. Previously in Jharkhand (India), the disease had affected a 25-day-old born. So what exactly is this deadly disease? Let's have a look at its causes, symptoms, treatment, and prevention.
What Is Necrotizing Fasciitis?
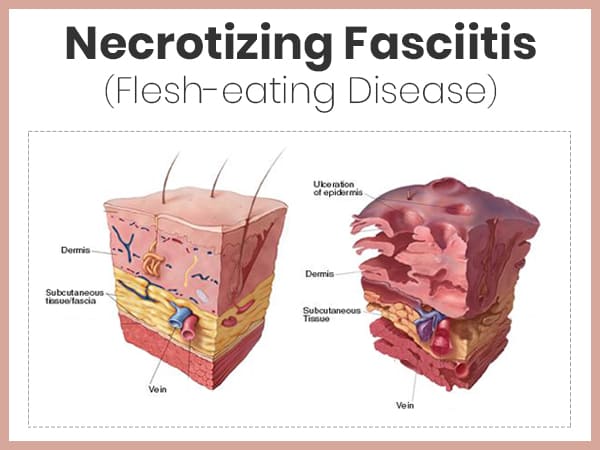
Necrotizing Fasciitis (NF) is a severe skin disease identified by the decaying infection of fasciae, connective tissues of the skin [1] . It is also known as flesh-eating disease which spreads rapidly on their host and causes the death of a person if not treated early. Only rapid antibiotic treatment or surgery can stop the infection from spreading.
There are several bacteria responsible for the spread of NF but medical experts believe that 'Group A Streptococcus' bacteria are highly responsible for the condition [2] . This lethal infection is believed to be affecting people since the fifth century BC during the time of Hippocrates. Earlier in the 18th century, it was known as 'phagedenic ulcer' as it destroys the surrounding tissues but later in the year 1952, this decaying disease was coined as necrotizing fasciitis and since then, its definition became broader. Also, every year in the US, around 500 cases of NF are noticed.

Types Of Bacteria Causing Necrotizing Fasciitis
There are several bacteria responsible for the spread of NF among which, some of the main ones are as follows:
- Group A Streptococci: As aforementioned, these Gram-positive bacteria are highly responsible for causing the disease. They are commonly present in the nose, skin, and throat of a person. Group A Streptococci bacteria are the one responsible for the cause of strep throat but when they get inside the skin through wounds, they start spreading and causes NF [2] .
- Vibrio vulnificus: These Gram-negative bacteria are found in marine environments like oceans, brackish ponds and estuaries. They enter through the injured skin or break in the skin while swimming in the infected water bodies[3] .
- Escherichia coli: These Gram-negative bacteria are found in the colon or large intestine. Sometimes, they are helpful as they restrict the entry of other bacteria in the intestine while in other scenarios, they harm us by causing food poisoning. In case the bacteria comes outside the intestine, they spread and cause NF [4] .
- Bacteroides: These Gram-negative bacteria are found mainly in the intestines, mouth, and genitals of a person. They usually benefit a human but in conditions like perforated bowel (hole in the walls of the intestine), mistakenly they come out and cause NF by entering through the skin injury [5] .
- Prevotella: These Gram-negative bacteria are present all over the body. When other NF-causing bacteria attacks the body, they add up to it and cause serious infection. Prevotella usually targets the neck, jaw, mouth, and face [6] .
Causes Of Necrotizing Fasciitis
NF is caused either by a single bacterium or more than one bacterium. These bacteria affect the connective tissues that lie beneath the skin. If a person has cut, wound, or external injury in their body, the bacteria find their way through these passages and enter the body of a person.
After entering the body, they spread through the tissues and while spreading, they produce two toxins (endotoxin and exotoxin) which obstruct the blood supply to the tissues. Due to this, tissues become impaired of blood supply which further restricts the passage of antibodies to the affected area. This causes the decaying of the tissues.
The infection spreads in four types which are as follows:
- Type 1 is spread by a combination of gram-positive cocci (like Group A Streptococci) [2] , gram-negative rods (Escherichia coli) [4] , and anaerobes (Bacteroides) bacteria [5]
- Type 2 is spread alone by Group A Streptococci
- Type 3 is spread by Vibrio vulnificus
- Type 4 is mainly fungal and caused by Candida
Granuloma Inguinale (Donovanosis): Symptoms, Stages, Causes & Treatment
Symptoms Of Necrotizing Fasciitis
The first symptoms of NF may be confusing as an infected person may get skin redness, muscle pull, or common flu symptoms. Slowly, the skin area will become painful and if there's a bump on the skin, it will start expanding and decaying. Other symptoms of NF include
- Fever with chills
- Low blood pressure [7]
- Vomiting
- Nausea
- Skin lesions like blisters and black dot [8]
- Extreme pain in the infection area
- Dizziness
- Fatigue
- Weakness
- Dehydration
- Diarrhoea
Risk Factors Of Necrotizing Fasciitis
Though NF can affect any individual, people who are at higher risk of the disease are as follows:
- Alcoholics or drug-consuming individuals [9]
- Older people
- Individuals with weak immunity
- Diabetics [10]
- Skin infection
- People with a chronic disease
- People who have undergone recent surgery
- Women during childbirth
- Obese people
Complications Of Necrotizing Fasciitis
The complications associated with NF are very serious and they include the following:
- Organ failure [11]
- Sepsis, a kind of blood infection
- Loss of limbs due to surgery of the large spread infection [12]
- Death
Diagnosis Of Necrotizing Fasciitis
The diagnosis of NF should be done as early as possible to prevent the spread of the infection and improve the survival rate of a person. Diagnosis of NF is carried out by the following tests:
- Laboratory blood testing to rule out other skin infections
- CT scan to see changes on the skin
- MRI to check for fascial thickening due to the infection
- Intra-operative biopsy to check for foul smell or bleeding loss by the bacteria [13]
- Tissue cultures on the infected body tissues
Treatment Of Necrotizing Fasciitis
The treatment of NF include the following therapies:
- Antibiotic therapy: The treatment helps control sepsis and restrict the spread of the infection. Antibiotics like vancomycin and daptomycin are recommended for the treatment.
- Surgical debridement: In this treatment, dead and infected tissues are removed to control the infection and let healthy tissues heal and grow more effectively. The treatment also works in preventing the infection from spreading to other organs [14] .
- Immune globulin (IVIG) therapy: Immunoglobulins are the antibodies found in animals which help fight against bacteria and viruses. The treatment is based on a concept that these antibodies can bind exo-toxins produced by the flesh-eating bacteria. However, the effectiveness of the treatment is still controversial.
- Hyperbaric oxygen therapy (HBO): This treatment method is used to inhibit the infection and exotoxin produced by them in hyperbaric conditions, exposing the wound to a 100% oxygen environment to speed up their healing. HBO is still controversial in treating NF.
How To Prevent Necrotizing Fasciitis
NF is not contagious. However, a person should take certain preventive measures. They are as follows:
- Clean all the minor cuts and injuries as soon as you get them.
- Don't go into swimming pools or water bodies with an open wound or any skin infection.
- Apply bandage to the injury to cover it.
- If there's a severe wound on your skin, consult a doctor immediately.
- If you are punctured by any marine creature like a stingray, get early medical assistance [15] .
- Be cautious of any fungal infection like athlete's foot.
- Avoid visiting marine areas where the disease occurrence is high.
- [1] 1. Sadasivan, J., Maroju, N. K., & Balasubramaniam, A. (2013). Necrotizing fasciitis. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India, 46(3), 472–478. doi:10.4103/0970-0358.121978
- [2] 2. Spellerberg, B., & Brandt, C. (2016). Laboratory diagnosis of Streptococcus pyogenes (group A streptococci). In Streptococcus pyogenes: Basic Biology to Clinical Manifestations [Internet]. University of Oklahoma Health Sciences Center.
- [3] 3. Phillips, K. E., & Satchell, K. J. (2017). Vibrio vulnificus: From Oyster Colonist to Human Pathogen. PLoS pathogens, 13(1), e1006053. doi:10.1371/journal.ppat.1006053
- [4] 4. Gallois, C., Hauw-Berlemont, C., Richaud, C., Bonacorsi, S., Diehl, J. L., & Mainardi, J. L. (2015). Fatal necrotizing fasciitis due to necrotic toxin-producing Escherichia coli strain. New microbes and new infections, 8, 109–112. doi:10.1016/j.nmni.2015.06.003
- [5] 5. Davies H. D. (2001). Flesh-eating disease: A note on necrotizing fasciitis. The Canadian journal of infectious diseases = Journal canadien des maladies infectieuses, 12(3), 136–140. doi:10.1155/2001/857195
- [6] 6. Gore M. R. (2018). Odontogenic necrotizing fasciitis: a systematic review of the literature. BMC ear, nose, and throat disorders, 18, 14. doi:10.1186/s12901-018-0059-y
- [7] 7. Tavares, R. L., Lafetá, P. N. Q., & Tôrres, P. A. C. (2018). Necrotizing Fasciitis following Laparoscopic Appendicecto-my: Case Report of Unpredict Surgical Site Complication. Ann Minim Invasive Surg, 1(1), 15-18.
- [8] 8. Patiño, J. F., & Castro, D. (1991). Necrotizing lesions of soft tissues: a review. World journal of surgery, 15(2), 235-239.
- [9] 9. Yii, Y. C., Hsieh, V. C., Lin, C. L., Wang, Y. C., & Chen, W. K. (2017). Alcohol use disorder increases the risk of necrotizing fasciitis: A nationwide retrospective cohort study. Medicine, 96(32), e7509. doi:10.1097/MD.0000000000007509
- [10] 10. Cheng, N. C., Tai, H. C., Chang, S. C., Chang, C. H., & Lai, H. S. (2015). Necrotizing fasciitis in patients with diabetes mellitus: clinical characteristics and risk factors for mortality. BMC infectious diseases, 15, 417. doi:10.1186/s12879-015-1144-0
- [11] 11. Smuszkiewicz, P., Trojanowska, I., & Tomczak, H. (2008). Late diagnosed necrotizing fasciitis as a cause of multiorgan dysfunction syndrome: A case report. Cases journal, 1(1), 125. doi:10.1186/1757-1626-1-125
- [12] 12. Misiakos, E. P., Bagias, G., Papadopoulos, I., Danias, N., Patapis, P., Machairas, N., … Machairas, A. (2017). Early Diagnosis and Surgical Treatment for Necrotizing Fasciitis: A Multicenter Study. Frontiers in surgery, 4, 5. doi:10.3389/fsurg.2017.00005
- [13] 13. Misiakos, E. P., Bagias, G., Patapis, P., Sotiropoulos, D., Kanavidis, P., & Machairas, A. (2014). Current concepts in the management of necrotizing fasciitis. Frontiers in surgery, 1, 36. doi:10.3389/fsurg.2014.00036
- [14] 14. Wong, C. H., Yam, A. K. T., Tan, A. B. H., & Song, C. (2008). Approach to debridement in necrotizing fasciitis. The American Journal of Surgery, 196(3), e19-e24.
- [15] 15. Charnigo, A., Thiele, G., & Ondrus, R. J. (2019). Stingray Sting. In StatPearls [Internet]. StatPearls Publishing.
-
 disorders cureFournier Gangrene: Causes, Symptoms, Risk factors, Treatment, And Prevention
disorders cureFournier Gangrene: Causes, Symptoms, Risk factors, Treatment, And Prevention -
 disorders cureDiabetes Drug Can Cause Flesh-Eating Genital Infection, New Study Reveals
disorders cureDiabetes Drug Can Cause Flesh-Eating Genital Infection, New Study Reveals -
 healthHow Dirty Is Your Phone? If Bacterias Could Speak They Would Have Said It Is Dirtier Than A Public Restroom!
healthHow Dirty Is Your Phone? If Bacterias Could Speak They Would Have Said It Is Dirtier Than A Public Restroom! -
 disorders cureRise In Antibiotic Resistance Among Indians Is The New Evolving Threat Amidst COVID-19 Pandemic: LANCET Study
disorders cureRise In Antibiotic Resistance Among Indians Is The New Evolving Threat Amidst COVID-19 Pandemic: LANCET Study -
 insyncAustralian Scientists Discover Superworms That Digest Styrofoam, Offering Hope For Plastic Waste Management
insyncAustralian Scientists Discover Superworms That Digest Styrofoam, Offering Hope For Plastic Waste Management -
 wellnessGerman Scientists Develop Bacterial Microrobots To Combat Cancer Without Any Pain And Tears
wellnessGerman Scientists Develop Bacterial Microrobots To Combat Cancer Without Any Pain And Tears -
 disorders cureMeningococcal Meningitis Outbreak In The US Has Killed A Quarter Of People: All About The Condition
disorders cureMeningococcal Meningitis Outbreak In The US Has Killed A Quarter Of People: All About The Condition -
 disorders cureTyphoid-Causing Bacteria Have Become Increasingly Resistant To Essential Antibiotics: Lancet Study
disorders cureTyphoid-Causing Bacteria Have Become Increasingly Resistant To Essential Antibiotics: Lancet Study -
 wellnessAMU Researchers Find 'Dangerous' Drug Resistant Bacterial Gene In Hospital Waste
wellnessAMU Researchers Find 'Dangerous' Drug Resistant Bacterial Gene In Hospital Waste -
 wellnessBacteria In Urine May Signal Aggressive Prostate Cancer: Study
wellnessBacteria In Urine May Signal Aggressive Prostate Cancer: Study -
 disorders cureWhat Are The Common Diseases Caused By Bacteria In Humans?
disorders cureWhat Are The Common Diseases Caused By Bacteria In Humans? -
 disorders cureWhat Is Typhoid Fever? Causes, Symptoms, Risk Factors, Complications, Treatments And Prevention
disorders cureWhat Is Typhoid Fever? Causes, Symptoms, Risk Factors, Complications, Treatments And Prevention


 Click it and Unblock the Notifications
Click it and Unblock the Notifications



